Complete Chapter 5
IOH ToolkitChapter 5. Simulation Learning
You’ve arrived at that point where it’s time to engage students and get them excited about oral health integration! The curriculum modules in this toolkit use multiple teaching methods so you can choose the ones that best match your educational preferences and the capabilities of your institution.
This chapter presents simulation learning, an innovative and flexible technique that immerses students in real-world scenarios. This method makes an excellent choice for interprofessional education because it allows students to practice communicating with other professionals and working as a team without putting patients at risk.
In this chapter you’ll find three sample simulations.
Simulation 1. Oral Examination and Dental Referral
Simulation 2. Oral Conditions and Speech
Simulation 3. Oral Health Risk Assessment
Chapter 5 Resources
All three simulations stand alone as independent lessons and most can be adapted to meet your particular needs. Each includes:
- At-a-Glance
- Instructor’s Guide
- Instructor’s Notes
- Case Scenarios
For more information regarding simulation learning, please see:
Simulation 1. Oral Examination and Dental Referral
Authors: Kristin Greenwood, PT, DPT, MS, GCS, Assistant Clinical Professor of Physical Therapy, and Alycia Markowski, PT, DPT, FAAOMT, OCS, Associate Clinical Professor of Physical Therapy, from the Department of Physical Therapy, Movement and Rehabilitation Sciences, Bouvé College of Heath Professions, Northeastern University.
At-a-Glance
| Topic | Oral examination and dental referral |
| Academic Focus | Clinical skills |
| Target IPEC Competencies | Domain: Values and Ethics
Work in cooperation with those who receive care, those who provide care, and others who contribute to or support the delivery of prevention and health services. |
| Target HRSA Competencies | Domain: Oral Health Evaluation
Perform oral health evaluations linking patient history, risk assessment, and clinical presentation. Domain: Interprofessional Collaborative Practice Exchange meaningful information among health care providers to identify and implement appropriate, high quality care for patients based on comprehensive evaluations and options available within the local health delivery and referral system. |
| Learning Objectives | Describe the health status of the patient’s teeth and gums. Identify abnormal lesions. Provide anticipatory guidance. Communicate appropriate referral, if needed, with appropriate time frame. |
Instructor’s Guide
Background information. This simulation was pilot tested with a group of Doctor of Physical Therapy students to integrate oral health evaluation and dental referral into a class session on temporomandibular joint (TMJ) disorders and treatment. Some of the exercises can be adapted for use with students of other health professions.
Overview for instructors. This simulation can be performed in any type of environment necessary (i.e., clinic, bedside, doctor’s office, or classroom). It
will allow students to practice an oral examination, provide patient education and recommendations, and make a dental referral.
Materials provided in this toolkit.
- Case Scenario 1, Case Scenario 2, and Case Scenario 3 with complete information for instructors and for actors portraying patients.
- Color photographs to illustrate each case scenario.
- Handouts for students:
Additional materials.
- Surgical mask
- Examination gloves
- 2×2 inch gauze
- Protective eyewear
Instructor preparation.
- Recruit one to three trained actors to play the role of patient. The number of actors you recruit will depend on how many students you are training.
- Review the patient case scenarios with the standardized patients.
- Practice the simulation with the standardized patients prior to the actual simulation.
- Assign students to interprofessional groups of five or six and create a simulation schedule that allows 40 minutes for each group to complete the exercise. It may be helpful to send students their group assignments and simulation schedules prior to the simulation.
- If available, recruit an additional faculty member who has oral health training or a dental provider to assist with the debriefing session.
Student preparation.
- Students should register for and complete the following Smiles for Life courses.
- Students should attend an in-class live demonstration of the oral examination once they have completed the Smiles for Life assignments.
- Students should review the case scenarios the week before the scheduled simulation.
Schedule.
- Live demonstration (15 minutes)
- Simulation orientation (3 minutes)
- Simulation (10 minutes)
- Debrief (10-12 minutes)
Instructor’s Notes
This simulation will take each group approximately 40 minutes to complete.
Live demonstration (15 minutes). To best prepare your students, perform a live demonstration of the oral exam before conducting the simulation. If time allows, consider teaching Workshop 1. The Oral Examination, located in Chapter 4. Faculty Development.
Simulation orientation (3 minutes). Review the learning objectives.
- Describe the health status of the patient’s teeth and gums.
- Identify abnormal lesions.
- Provide anticipatory guidance.
- Communicate the appropriate referral (if needed) within the appropriate time frame.
Review the simulation process with the students.
- State the length of the simulation (10 minutes).
- Point out the location of the surgical masks, gloves, gauze, and protective eyewear students will need.
- Provide each student with a copy of the Provider Notes Worksheet and the Sample Dental Referral Form. Instruct students to fill out these forms during the simulation.
- Ask each group to pick a student to play the role of provider. All other students in the group will observe.
- Remind students that only the provider will interact with the patient.
Simulation (10 minutes).
- Role of provider. The provider in each group will interact with the standardized patient while the other students observe. The provider interacts with the standardized patient as if that person had the clinical condition outlined in the case scenario and presented in the accompanying photographs. The provider will:
- View a photograph of the presenting clinical condition for the case.
- Offer the patient anticipatory guidance based on the clinical findings in the photograph.
- Make a dental referral using the Sample Dental Referral Form if appropriate.
The provider should refer to the Critical Items Checklist for Simulation 1 and complete the Provider Notes Worksheet during the clinical encounter.
- Role of observer. The observers in each group will watch their classmate interact with the patient and make their own independent decisions regarding recommendations and referral. Observers should refer to the Critical Items Checklist for Simulation 1 during the simulation and complete both the Provider Notes Worksheet and the Sample Dental Referral Form. Observers should not communicate with one another, the provider, or the patient during the simulation.
Debrief (10 – 12 minutes). After each simulation, generate open discussion about the exercise by inviting reactions from both the standardized patient(s) and the students. To begin discussion, review the questions included on the Provider Notes Worksheet.
For further prompting, you can ask the students to consider the patient history and specific clinical findings as they relate to the following questions.
- How would you describe the health status of the patient’s teeth and gums?
- If you found a lesion, would you classify it as normal or abnormal based on the patient history and the clinical examination?
- What did you think of the anticipatory guidance the provider offered the patient? Would you have offered anything different?
- Would you refer the patient to a dental provider? If so, why?
Case Scenario 1 (Instructor/Actor Copy)
You are a physical therapist. A patient comes to you complaining of headaches and jaw pain.
Patient information.
Name: Alex
Age: 21
Occupation: Student
Reason for visit: Headaches and jaw pain due to previously diagnosed TMJ dysfunction.
As her physical therapist, you decide to perform an oral examination and make several observations.
Alex reports that she has not seen a dentist since starting college because she does not know any local dentists. An oral examination reveals red and swollen gums with moderate to heavy plaque accumulation.

Photo: public domain
- Brush twice daily with a soft bristled toothbrush.
- Floss once daily.
- Use a fluoride mouth rinse at night to help reduce plaque and bacteria.
Alex should receive a dental referral from the provider before she leaves.
Case Scenario 2 (Instructor/Actor Copy)
You are a physical therapist. A patient comes to you complaining of headaches and jaw pain.
Patient information.
Name: Alex
Age: 21
Occupation: Student
Reason for visit: Headaches and jaw pain due to previously diagnosed temporomandibular joint (TMJ) dysfunction.
As her physical therapist, you decide to perform an oral examination and make several observations.
Alex is unable to open her mouth completely and has a large red bump on her gums, right under one of her back teeth. The tooth looks like there is a cavity present. Alex reports the area is very painful and won’t stop throbbing.
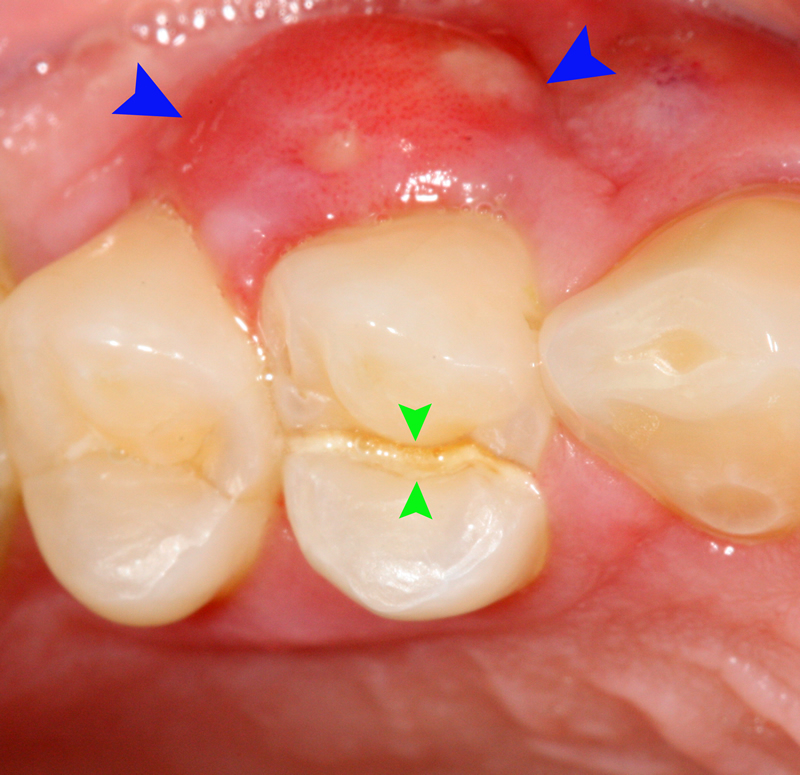
Case Scenario 3 (Instructor/Actor Copy)
You are a physical therapist. A patient comes to you complaining of headaches and jaw pain.
Patient information.
Name: Alex
Age: 21
Occupation: Student
Reason for visit: Headaches and jaw pain due to previously diagnosed temporomandibular joint (TMJ) dysfunction.
As her physical therapist, you decide to perform an oral examination and make several observations.
Alex reports that she smokes about a pack of cigarettes a week and has done so for the past four years. During the examination, you find a white and red lesion on the base of Alex’s tongue. Alex says she noticed the lesion about a month ago but didn’t think it was a big deal.
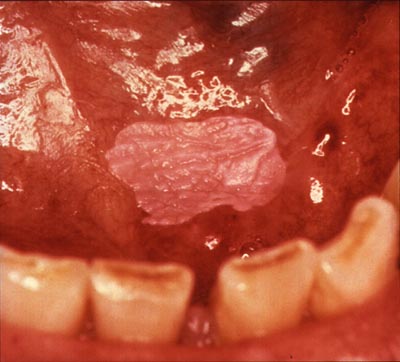
Photo: public domain
Simulation 2. Oral Conditions and Speech
Author: Emily Zimmerman, PhD, CCC-SLP, Assistant Professor, Department of Communication Sciences and Disorders, Bouvé College of Heath Sciences, Northeastern University.
At-a-Glance
| Topic | Oral conditions and speech |
| Academic Focus | Clinical skills |
| Target IPEC Competencies | Domain: Roles and Responsibilities
Engage diverse healthcare professionals who complement one’s own professional expertise, as well as associated resources, to develop strategies to meet specific patient care needs. |
| Target HRSA Competencies | Domain: Oral Health Evaluation
Identify and prioritize strategies to prevent or mitigate risk for oral and systemic diseases. Domain: Interprofessional Collaborative Practice Apply interprofessional practice principles that lead to safe, timely, efficient, effective, equitable planning and delivery of patient and population-centered oral health care. |
| Learning Objectives | Promote an in-depth understanding of how dentistry and speech-language pathology both play a vital role in oral health and how one profession greatly influences the other. |
Instructor’s Guide
Background information. This simulation was pilot tested with a group of undergraduate speech-language pathology and audiology (SLPA) and dental students in years 1–3 of their program. This simulation is designed to help SLPA and dental students work together to understand the impact of common oral conditions on speech and speech development. Some of the exercises can be adapted for use with students of other health professions.
Overview for instructors. This simulation can be performed in any type of environment necessary (i.e., clinic, bedside, doctor’s office, or classroom). It allows SLPA and dental students to work together with the common goal of exchanging clinically relevant information so they may identify and implement appropriate care for patients suffering from common oral conditions.
As part of the simulation, three-dimensional tooth models representing various oral conditions were used, but if these are not available, photographs will suffice.
Materials provided in this toolkit.
- Case Scenario 1, Case Scenario 2, and Case Scenario 3 with complete information for instructors and for actors portraying patients.
- Handouts for students:
Additional materials.
- Three dimensional models (optional)
Instructor preparation.
- Recruit one to three trained actors to play the role of patient. The number of actors you recruit will depend on how many students you are training.
- Review the patient case scenarios with the standardized patients.
- Practice the simulation with the standardized patients prior to the actual simulation.
- Partner with dental faculty to recruit dental students who will work with the other students during the simulation to identify the oral condition and the course of action.
- Ask a faculty member from each of the programs participating in the simulation to locate or draft a short description of the roles and responsibilities for his or her profession. Compile these descriptions into one Word document and make it available to your students through email, your preferred learning management system, or your website.
- Refer to your roster and break students into groups of five or six before the day of the simulation. If possible, assign at least one dental student to each group.
Student preparation.
- Students should register for and complete the following Smiles for Life courses.
- Most SLPA students learn about oral mechanisms exams as part of their speech-language pathology criteria. However, if this is new information there is an abundance of online resources that can help to inform the student about this procedure.
- Students should review the roles and responsibilities document provided by the instructor prior to the simulation.
Schedule.
- Simulation orientation (5 minutes)
- Simulation (30 minutes)
Instructor’s Notes
This simulation will take each group of students approximately 35 minutes to complete.
Simulation orientation (5 minutes). Review learning objectives.
- Promote an in-depth understanding of how dentistry and speech-language pathology and audiology together contribute to oral health.
- Demonstrate how each of these professions influences the other.
Review the simulation process with the students.
- State the length of the simulation (35 minutes).
- Give each student a copy of Case Scenario 1.
- Explain the purpose of the three-dimensional models or photographs.
- Explain that students will break into pre-assigned teams and work together to complete the simulations.
- Note that groups should spend about 10 minutes on each patient case.
Simulation (30 minutes).
One standardized patient will work with each team to act out the three scenarios: (1) Acute dental injury that resulted in missing teeth, (2) ankyloglossia, and (3) tongue thrusting. A three-dimensional dental model or photographs representing the dental problem will accompany each scenario.
To conduct the simulation, teams should take the following steps.
- Enter the room as a team and interact with the standardized patient to determine what brought him or her into the office.
- Listen to the patient’s concerns, then examine the three-dimensional dental model or photographs together.
- Consider the patient’s history along with the clinical evidence found during the examination to assess the case.
- Document findings in real-time. Each team member should take his or her own notes.
- Consult with one another on findings and designate one team-member to report to the patient.
- Report findings to the patient and recommend a plan of treatment.
Case Scenario 1 (Instructor/Actor Copy)
You are a speech-language pathologist. A patient comes to you complaining of headaches and jaw pain.
Patient information.
Name: Tim
Age: 18
Occupation: Student
Reason for visit: Tim’s friends cannot understand him when he talks.
Background information. Tim has no other known medical complaints. Two weeks ago, Tim’s front wheel locked while he was riding his bike, throwing him over the handlebars. Tim landed face first on the pavement. He did not suffer any serious neck or back injuries.
Chief concern. When Tim fell off of his bike, he hit his mouth and is now missing three front teeth.
Dental consequences. Missing central incisors, as well as right lateral incisor. Loss of alveolar bone leading to collapse of lower facial 1/3 and mesial drift of right canine (#6) and left lateral incisor (#10).
Note: Dental faculty should be prepared to explain this terminology to the SPLA students.
Speech consequences. Reduced intelligibility. Tim has trouble correctly producing some phonemes. These include /s/, /θ/, /v/, and likely all alveolar sounds.
Note: SPLA faculty should be prepared to explain this terminology to the dental students.
Recommendations. An immediate consult and examination by a dentist is needed to address missing teeth and injury to surrounding tissues. The patient should also work with a speech-language pathologist to address speech development problems resulting from the accident.
Photographs. Top photographs are of three-dimensional models. The bottom photograph shows an actual clinical representation.

Photo: Emily Zimmerman, PhD, CCC-SLP, Assistant Professor, Department of Communication Sciences and Disorders, Bouvé College of Heath Sciences, Northeastern University.

Photo: iStock.com/Ugur Atila
- What is the patient’s chief concern?
- What are the dental consequences of the patient’s oral condition?
- What are the speech consequences of the patient’s oral condition?
- What are your recommendations for this patient?
Case Scenario 2 (Instructor/Actor Copy)
You are a speech-language pathologist. A patient comes to you complaining of headaches and jaw pain.
Patient information.
Name: Michael
Age: 3
Occupation: Minor
Reason for visit: Michael’s mother is having trouble understanding his speech.
Background information. Michael was born with a short frenulum. His mother reports that she can only understand about half of what her son says. She also reports he had some difficulty sucking as an infant.
Chief concern. Michael has difficulty sucking, getting milk from a bottle, and licking, such as with an ice cream cone. It is also hard to understand him when he speaks.
Dental consequences. Ankyloglossia, lingual gingival recession, and diastema between mandibular central incisors (tooth numbers 25 and 26).
Note: Dental faculty should be prepared to explain this terminology to the SPLA students.
Speech consequences. Michael also has difficulty producing /t/, /d/, /n/, and /l/.
Overall health consequences. Michael has difficulty consuming certain foods.
Recommendations. Michael should be referred to a dentist to see if he is eligible to have his frenulum clipped. This would extend the length of his tongue and address his difficulties. If his speech problems do not resolve after his frenulum is clipped, Michael should work with a speech-language pathologist.
Photographs. Top photographs are of three-dimensional models. The bottom photograph shows an actual clinical representation.

Photo: Emily Zimmerman, PhD, CCC-SLP, Assistant Professor, Department of Communication Sciences and Disorders, Bouvé College of Heath Sciences, Northeastern University.

- What is the patient’s chief concern?
- What are the dental consequences of the patient’s oral condition?
- What are the speech consequences of the patient’s oral condition?
- What are your recommendations for this patient?
Case Scenario 3 (Instructor/Actor Copy)
You are a speech-language pathologist. A patient comes to you complaining of headaches and jaw pain.
Patient information.
Patient name: Sally
Age: 10
Occupation: Student
Reason for visit: Sally’s dentist will not apply braces until her tongue thrust is resolved.
Background information. Sally demonstrates a tongue thrust when she swallows. Her dentist says she needs braces, but her orthodontist will not put braces on until the tongue thrust is resolved. The orthodontist has explained that if the tongue thrust continues after the braces are removed, pressure from the tongue could move Sally’s teeth forward again.
Chief concern. Sally needs braces but can’t have them placed until she stops thrusting her tongue.
Dental consequences. Sally’s tongue thrust has pushed her top central incisors forward. This has caused an anterior open bite, protrusion, and rotation of the central incisors.
Note: Dental faculty should be prepared to explain this terminology to the SPLA students.
Speech consequences. Sally has difficulty producing /s/, /z/, “ch”, “sh”, and “zh.”
Recommendations. Sally’s dentist should refer her to a speech-language pathologist to address her tongue thrusting habit. The dentist and speech-language pathologist should collaborate to address this problem.
Photographs. Top photographs are of three-dimensional models. The bottom photograph shows an actual clinical representation.

Photo: Emily Zimmerman, PhD, CCC-SLP, Assistant Professor, Department of Communication Sciences and Disorders, Bouvé College of Heath Sciences, Northeastern University.

- What is the patient’s chief concern?
- What are the dental consequences of the patient’s oral condition?
- What are the speech consequences of the patient’s oral condition?
- What are your recommendations for this patient?
Simulation 3. Oral Health Risk Assessment
Authors: Pooja Bhalla, MSN, RN, Adjunct Faculty, School of Nursing, Bouvé College of Health Sciences, Northeastern University and Colleen Anderson, DDS, Associate Dental Director, Boston Health Care for the Homeless Program.
At-a-Glance
| Topic | Oral health risk assessment |
| Academic Focus | Clinical skills |
| Target IPEC Competencies | Domain: Roles and Responsibilities
Engage diverse healthcare professionals who complement one’s own professional expertise, as well as associated resources, to develop strategies to meet specific patient care needs. |
| Target HRSA Competencies | Domain: Risk Assessment
Conduct patient-specific, oral health risk assessments on all patients. Domain: Communication and Education Provide targeted patient education about importance of oral health and how to maintain good oral health, which considers oral health literacy, nutrition, and patient’s perceived oral health barriers. |
| Learning Objectives | Describe the impact of oral health on systemic health and chronic disease management. Identify risk factors that impact oral health. Identify and describe the impact of risky behaviors on oral health. |
Instructor’s Guide
Background. This simulation was pilot tested with a group of case managers, medical assistants, and respite aides in a patient-centered medical home (a primary care practice that has adopted a set of practices aimed at coordinating and improving the delivery of patient care). This simulation can be adapted for use with students of any health profession.
Overview for instructors. The purpose of this exercise is to provide health professions students the opportunity to interview a patient, make an oral health risk assessment, and determine the need for referral. This simulation does not incorporate an oral examination as part of the risk assessment. It can be performed in any type of environment necessary (i.e., clinic, bedside, doctor’s office, or classroom).
Materials provided in this toolkit.
- Case Scenario 1 and Case Scenario 2 with complete information for instructors and for actors portraying patients.
- Handouts for students:
Additional materials.
- None
Instructor preparation.
- Recruit one or two trained actors to play the role of patient. The number of actors you recruit will depend on how many students you are training.
- Review the patient case scenarios with the standardized patients.
- Practice the simulation with the standardized patients prior to the actual simulation.
- Assign students to groups of five or six and create a simulation schedule that allows 30 minutes for each group to complete the exercise. It may be helpful to send students their group assignments and simulation schedules prior to the simulation.
Student preparation.
- Students should register for and complete the following Smiles for Life courses.
- Course 1: The Relationship of Oral-Systemic Health
- Course 3: Adult Oral Health
- Students should review the ADA Caries Risk Assessment Form (Age>6) contained in this toolkit.
Schedule.
- Simulation orientation (5 minutes)
- Simulation (15 minutes)
- Debrief (10 minutes)
Instructor’s Notes
This simulation will take approximately 30 minutes for each group of students to complete.
Simulation orientation (5 minutes). Review learning objectives.
- Describe the impact of oral health on systemic health and chronic disease management.
- Identify risk factors that impact oral health.
- Identify and describe the impact of alcohol use, tobacco use, or other risky behaviors on oral health.
Review the simulation process with the students.
- State the length of the simulation (30 minutes).
- Review the ADA Caries Risk Assessment Form Age >6 and the Dental Referral Form.
- Explain that one student in each group will act as the provider and all other students in the group will act as observers.
- Emphasize that only the provider will interact with the patient while all other students observe.
Simulation (15 minutes).
- Role of provider. The provider in each group will interact with the patient by reading from a script while the other students observe. After the standardized patient presents with findings outlined in his or her patient case scenario, the provider will:
- View a photograph of the presenting clinical condition the patient described.
- Complete the ADA Caries Risk Assessment Form Age >6.
- Offer the patient anticipatory guidance based on the clinical findings in the photograph.
- Make a dental referral using the Dental Referral Form if necessary.
The provider should refer to the Critical Items Checklist for Simulation 3 throughout the clinical encounter.
- Role of student observers. The observers should watch the provider interact with the patient and read along with the script as the interview progresses. Observers should make independent decisions regarding assessment, recommendations, and referral while filling out their own copies of the ADA Caries Risk Assessment and the Dental Referral Forms. Observers should not communicate during the simulation.
The observers should refer to the Critical Items Checklist throughout the clinical encounter.
Debrief (10 minutes). Generate open discussion about the simulation by inviting reactions from both the standardized patient and the students. To prompt discussion, ask students to consider the given patient history and specific clinical findings. Then ask debriefing questions.
- How did you classify the patient’s risk status (low, moderate, high)?
- What specific recommendations did you have for this patient?
- What did you think of the anticipatory guidance the provider offered the patient? Would you have offered anything different?
- Would you refer the patient to a dental provider? If so, why?
Case Scenario 1 (Instructor/Actor Copy)
Patient information.
Name: Veronica
Age: 45
Setting: Medical triage
Chief concern: Patient wants to discuss her diabetes. Her blood sugar levels have been high.
Medical History:
- Type 2 diabetes mellitus
- History of alcohol abuse but not currently using
- High blood pressure
- No other general health conditions
Script. As part of her appointment, you decide to address the patient’s oral health.
Provider: Do you see a dentist?
Patient: I don’t right now.
Provider: Do you drink tap water or bottled water?
Patient: I don’t drink much water, but if I do it’s through the tap.
Provider: Do you use toothpaste with fluoride in it?
Patient: I guess. I just buy what’s on sale at the store, and I try to brush everyday. Sometimes I forget. I don’t floss because it makes my gums bleed.
Provider: How often do you eat or drink sugary foods?
Patient: I drink coffee throughout the day with regular sugar. Sugary foods once in a while.
Provider: Do you have any mouth pain?
Patient: Sometimes. My gums get sore, and I bleed when I brush.
Provider: How intense and frequent is the pain?
Patient: It’s not sharp, it feels like throbbing, every time after I brush.
Provider: Do you wear dentures?
Patient: No. I don’t have any teeth missing.
Provider: Do you experience dry mouth?
Patient: Not that I’m aware of.
Provider: Do you smoke or use tobacco products?
Patient: Yes. I smoke cigarettes.
Provider: How many a day?
Patient: About half a pack.
Provider: Are you interested in cutting down or quitting?
Patient: No. Not now.

Photo: public domain
- Summary. The presence of diabetes places Veronica at a high risk for gum disease. Her history of alcohol abuse and current smoking habit also place her at an automatic high risk for tooth decay and oral cancer. Further contributing to her risk of tooth decay is her lack of proper oral hygiene and consumption of coffee with sugar throughout the day. The photograph reveals heavy plaque buildup and inflamed gums.
- ADA Caries Risk Assessment. Veronica is at moderate to high risk for caries due to little fluoride exposure, exposure to sugary drinks throughout the day, lack of a dental home, and visible plaque. These findings demonstrate that the provider does not need to address every category of the ADA Caries Risk Assessment to determine the patient needs a dental referral.
- Patient specific recommendations. Refer Veronica to a dental provider for a comprehensive evaluation. Recommend she drink more water throughout the day, use toothpaste with fluoride while brushing twice a day, floss everyday, replace the sugar in her coffee with an artificial sweetener, and smoke less. Educate Veronica on the connection between diabetes and gum disease. If she is interested, provide Veronica with information about services that might help her quit smoking.
Case Scenario 2 (Instructor/Actor Copy)
Patient information.
Name: Vance
Age: 57
Setting: Primary care clinic
Chief concern: Follow-up visit after receiving new medications for high blood pressure and depression
Medical history:
- High blood pressure (taking medication)
- Depression (taking medication)
- No other general health conditions
Script. As part of Vance’s appointment, you decide to address his oral health.
Provider: When was the last time you visited a dentist?
Patient: I had dentures made about a year ago to replace some teeth that got pulled, and I haven’t been since because the office is far and hard to get to.
Provider: How are your dentures fitting?
Patient: Pretty good, but sometimes I have trouble eating because they rub against my gums.
Provider: Do you take your dentures out at night?
Patient: Yes, because my mouth is really dry and it feels good to my gums when I take out my dentures.
Provider: How often do you get dry mouth, and what do you do about it?
Patient: Pretty often since I started the medications. To help I’ll drink something refreshing like lemonade or a sprite.
Provider: How often do you drink lemonade or sprite?
Patient: I like to sip on it during the day while I work or watch television.
Provider: How many times a day do you brush and floss?
Patient: I brush twice a day, I floss every once in a while. I try to be better about it.
Provider: Do you smoke or use tobacco products?
Patient: Yes, I smoke.
Provider: How often?
Patient: About seven or eight a day.
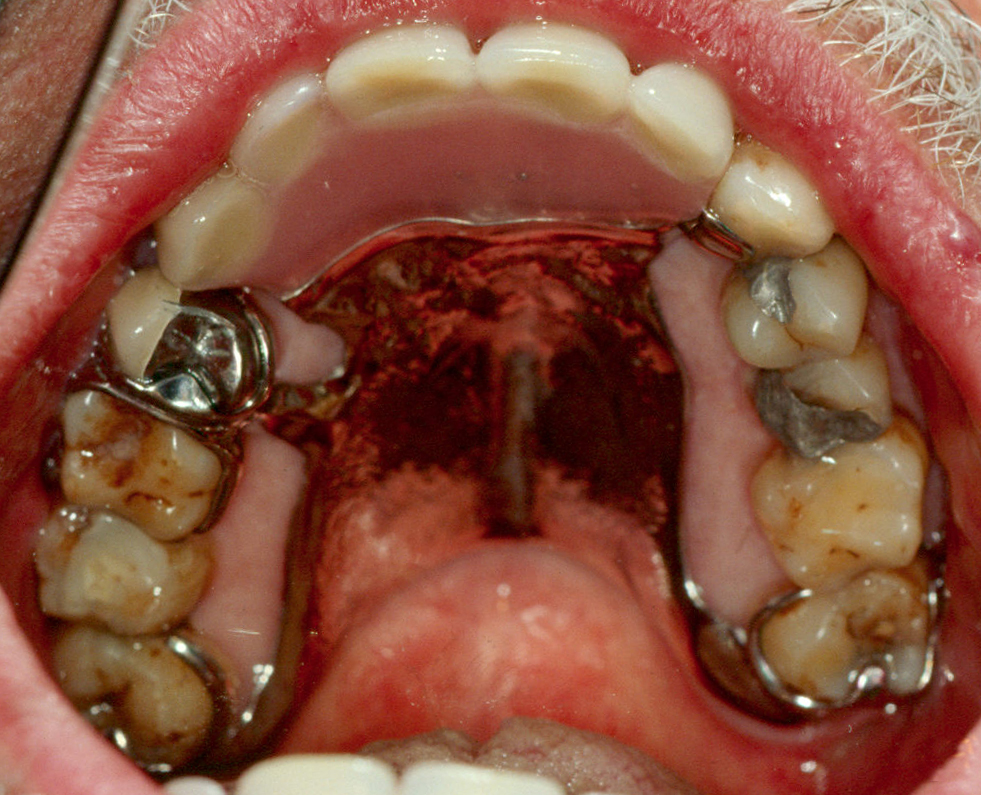
Photo: public domain

- Summary. The fact that Vance has removable dentures to replace pulled teeth indicates a history of oral disease and places him at high risk for dental caries (tooth decay). His medications are causing dry mouth, which is a common side effect. This also places him at an increased risk for dental caries. The patient’s consumption of sugary drinks and use of cigarettes only worsens his dry mouth and further increases his risk of decay. The photograph shows very dry mouth and fissured tongue.
- ADA Caries Risk Assessment. Vance is at high risk for caries due to exposure to sugary drinks throughout the day, lack of a regular dental home, and a recent history of tooth decay. These findings demonstrate the provider does not need to address every category of the ADA Caries Risk Assessment to determine the patient needs a dental referral.
- Patient specific recommendations. Refer Vance to a dental provider for a comprehensive examination and consultation regarding his dentures, the consequences of dry mouth (caries), and information about how to prevent dry mouth. Recommend flossing and a fluoride rinse. If he is interested, provide Vance with information about services that might help him quit smoking.
Chapter 5 Resources
- ADA Caries Risk Assessment Form (>6)
- ADA Caries Risk Assessment Instructions
- Provider Notes Worksheet
- Sample Dental Referral Form
- Simulation 1, Case Scenario 1
- Simulation 1, Case Scenario 2
- Simulation 1, Case Scenario 3
- Simulation 1, Critical Items Checklist
- Simulation 2, Case Scenario 1
- Simulation 2, Case Scenario 2
- Simulation 2, Case Scenario 3
- Simulation 3, Case Scenario 1
- Simulation 3, Case Scenario 2
- Simulation 3, Critical Items Checklist


