Simulation 1. Oral Examination and Dental Referral
IOH ToolkitChapter 5. Simulation Learning
Simulation 1. Oral Examination and Dental Referral
Authors: Kristin Greenwood, PT, DPT, MS, GCS, Assistant Clinical Professor of Physical Therapy, and Alycia Markowski, PT, DPT, FAAOMT, OCS, Associate Clinical Professor of Physical Therapy, from the Department of Physical Therapy, Movement and Rehabilitation Sciences, Bouvé College of Heath Professions, Northeastern University.
At-a-Glance
| Topic | Oral examination and dental referral |
| Academic Focus | Clinical skills |
| Target IPEC Competencies | Domain: Values and Ethics
Work in cooperation with those who receive care, those who provide care, and others who contribute to or support the delivery of prevention and health services. |
| Target HRSA Competencies | Domain: Oral Health Evaluation
Perform oral health evaluations linking patient history, risk assessment, and clinical presentation. Domain: Interprofessional Collaborative Practice Exchange meaningful information among health care providers to identify and implement appropriate, high quality care for patients based on comprehensive evaluations and options available within the local health delivery and referral system. |
| Learning Objectives | Describe the health status of the patient’s teeth and gums. Identify abnormal lesions. Provide anticipatory guidance. Communicate appropriate referral, if needed, with appropriate time frame. |
Instructor’s Guide
Background information. This simulation was pilot tested with a group of Doctor of Physical Therapy students to integrate oral health evaluation and dental referral into a class session on temporomandibular joint (TMJ) disorders and treatment. Some of the exercises can be adapted for use with students of other health professions.
Overview for instructors. This simulation can be performed in any type of environment necessary (i.e., clinic, bedside, doctor’s office, or classroom). It
will allow students to practice an oral examination, provide patient education and recommendations, and make a dental referral.
Materials provided in this toolkit.
- Case Scenario 1, Case Scenario 2, and Case Scenario 3 with complete information for instructors and for actors portraying patients.
- Color photographs to illustrate each case scenario.
- Handouts for students:
Additional materials.
- Surgical mask
- Examination gloves
- 2×2 inch gauze
- Protective eyewear
Instructor preparation.
- Recruit one to three trained actors to play the role of patient. The number of actors you recruit will depend on how many students you are training.
- Review the patient case scenarios with the standardized patients.
- Practice the simulation with the standardized patients prior to the actual simulation.
- Assign students to interprofessional groups of five or six and create a simulation schedule that allows 40 minutes for each group to complete the exercise. It may be helpful to send students their group assignments and simulation schedules prior to the simulation.
- If available, recruit an additional faculty member who has oral health training or a dental provider to assist with the debriefing session.
Student preparation.
- Students should register for and complete the following Smiles for Life courses.
- Students should attend an in-class live demonstration of the oral examination once they have completed the Smiles for Life assignments.
- Students should review the case scenarios the week before the scheduled simulation.
Schedule.
- Live demonstration (15 minutes)
- Simulation orientation (3 minutes)
- Simulation (10 minutes)
- Debrief (10-12 minutes)
Instructor’s Notes
This simulation will take each group approximately 40 minutes to complete.
Live demonstration (15 minutes). To best prepare your students, perform a live demonstration of the oral exam before conducting the simulation. If time allows, consider teaching Workshop 1. The Oral Examination, located in Chapter 4. Faculty Development.
Simulation orientation (3 minutes). Review the learning objectives.
- Describe the health status of the patient’s teeth and gums.
- Identify abnormal lesions.
- Provide anticipatory guidance.
- Communicate the appropriate referral (if needed) within the appropriate time frame.
Review the simulation process with the students.
- State the length of the simulation (10 minutes).
- Point out the location of the surgical masks, gloves, gauze, and protective eyewear students will need.
- Provide each student with a copy of the Provider Notes Worksheet and the Sample Dental Referral Form. Instruct students to fill out these forms during the simulation.
- Ask each group to pick a student to play the role of provider. All other students in the group will observe.
- Remind students that only the provider will interact with the patient.
Simulation (10 minutes).
- Role of provider. The provider in each group will interact with the standardized patient while the other students observe. The provider interacts with the standardized patient as if that person had the clinical condition outlined in the case scenario and presented in the accompanying photographs. The provider will:
- View a photograph of the presenting clinical condition for the case.
- Offer the patient anticipatory guidance based on the clinical findings in the photograph.
- Make a dental referral using the Sample Dental Referral Form if appropriate.
The provider should refer to the Critical Items Checklist for Simulation 1 and complete the Provider Notes Worksheet during the clinical encounter.
- Role of observer. The observers in each group will watch their classmate interact with the patient and make their own independent decisions regarding recommendations and referral. Observers should refer to the Critical Items Checklist for Simulation 1 during the simulation and complete both the Provider Notes Worksheet and the Sample Dental Referral Form. Observers should not communicate with one another, the provider, or the patient during the simulation.
Debrief (10 – 12 minutes). After each simulation, generate open discussion about the exercise by inviting reactions from both the standardized patient(s) and the students. To begin discussion, review the questions included on the Provider Notes Worksheet.
For further prompting, you can ask the students to consider the patient history and specific clinical findings as they relate to the following questions.
- How would you describe the health status of the patient’s teeth and gums?
- If you found a lesion, would you classify it as normal or abnormal based on the patient history and the clinical examination?
- What did you think of the anticipatory guidance the provider offered the patient? Would you have offered anything different?
- Would you refer the patient to a dental provider? If so, why?
Case Scenario 1 (Instructor/Actor Copy)
You are a physical therapist. A patient comes to you complaining of headaches and jaw pain.
Patient information.
Name: Alex
Age: 21
Occupation: Student
Reason for visit: Headaches and jaw pain due to previously diagnosed TMJ dysfunction.
As her physical therapist, you decide to perform an oral examination and make several observations.
Alex reports that she has not seen a dentist since starting college because she does not know any local dentists. An oral examination reveals red and swollen gums with moderate to heavy plaque accumulation.

Photo: public domain
- Brush twice daily with a soft bristled toothbrush.
- Floss once daily.
- Use a fluoride mouth rinse at night to help reduce plaque and bacteria.
Alex should receive a dental referral from the provider before she leaves.
Case Scenario 2 (Instructor/Actor Copy)
You are a physical therapist. A patient comes to you complaining of headaches and jaw pain.
Patient information.
Name: Alex
Age: 21
Occupation: Student
Reason for visit: Headaches and jaw pain due to previously diagnosed temporomandibular joint (TMJ) dysfunction.
As her physical therapist, you decide to perform an oral examination and make several observations.
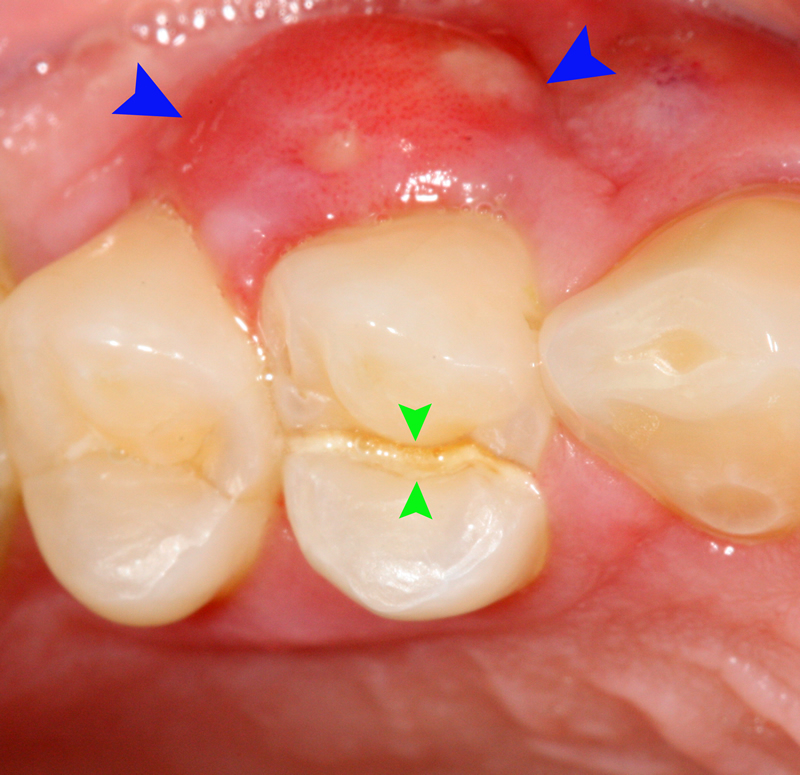
Alex is unable to open her mouth completely and has a large red bump on her gums, right under one of her back teeth. The tooth looks like there is a cavity present. Alex reports the area is very painful and won’t stop throbbing.
Case Scenario 3 (Instructor/Actor Copy)
You are a physical therapist. A patient comes to you complaining of headaches and jaw pain.
Patient information.
Name: Alex
Age: 21
Occupation: Student
Reason for visit: Headaches and jaw pain due to previously diagnosed temporomandibular joint (TMJ) dysfunction.
As her physical therapist, you decide to perform an oral examination and make several observations.
Alex reports that she smokes about a pack of cigarettes a week and has done so for the past four years. During the examination, you find a white and red lesion on the base of Alex’s tongue. Alex says she noticed the lesion about a month ago but didn’t think it was a big deal.
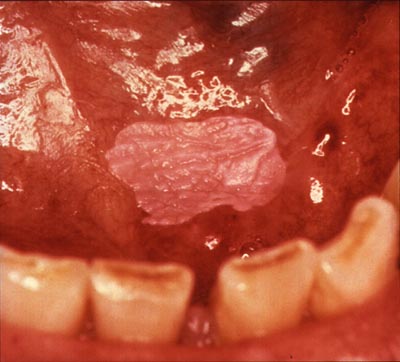
Photo: public domain
First Published: 11/2015
Last updated: 03/2016


